Ultrasound- Guided Interscalene Brachial Plexus Block
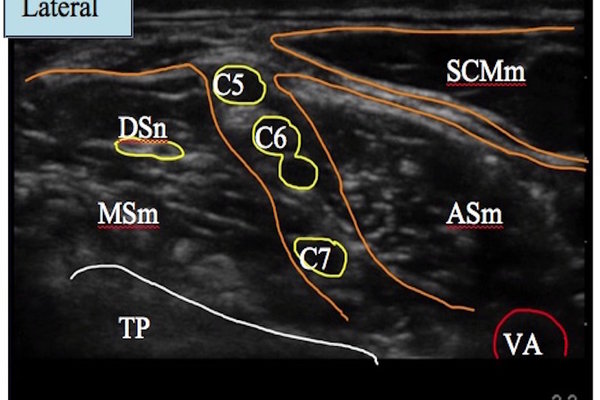
Nerves Blocked: Nerve Roots C5,C6,C7
Location: Interscalene groove (between anterior and middle scalene muscles)
Difficulty: Green/ Blue
Indications: Shoulder and proximal humerus surgery
Patient Position: Supine, head to face opposite side
Needle: 50mm short beveled regional block needle
Probe: High frequency linear
Tiger Territory: Vertebral artery (often in close proximity to C7 nerve root)
Carotid artery & internal jugular vein
Phrenic nerve (on surface anterior scalene muscle)
Think Twice if: Contralateral pneumothorax/ phrenic nerve palsy/ pneumonectomy
Severe respiratory disease eg.COPD
Interscalene block already in opposite side
Image Optimisation: Screen depth 1-2cm
Identify brachial plexus behind the subclavian artery & trace proximally
Or identify the structures as the probe is slid laterally from midline.
Slight caudad intent of probe may help
Key: C5, C6, C7 nerve roots
TP- transverse process, MSm- Middle scalene muscle, ASm- Anterior scalene muscle, SCMm-Sternocleidomastoid muscle, VA-Vertebral artery, DSn- Dorsal scapular nerve
Needling: In-plane (IP) or out-of-plane (OOP)
IP
Ø Better visibility of needle/nerve interface.
OOP
Ø More comfortable (shorter needle path)
Ø Avoid risk of damage to dorsal scapular or long thoracic nerves (in middle scalene muscle)
Ø Ideal for perineural catheter placement.
Deposit local anaesthetic to surround C5 & C6 nerve roots
Complications/SEs: Phrenic nerve block, hence caution in respiratory disease
Horner’s syndrome (stellate ganglion block)
Recurrent laryngeal nerve block
Vertebral artery puncture/injection
Spinal/ epidural injection
Pearls: Plexus at this level appears as a string of hypoechoic circles (“traffic lights”)
Superficial block- usually nerve roots 1-2cm from skin
C6 root often divides into two structures (“double bubble” appearance)
Use colour doppler to identify vascular structures, especially the vertebral artery
Nerve roots can be traced back to their intervertebral foramen to aid identification
Vertebral transverse processes (TP) have characteristic appearances
Ø C5 TP bifid with large posterior tubercle
Ø C6 TP bifid with large anterior tubercle (Chassaignac’s)
Ø C7 TP has no anterior tubercle.
Use lower volumes to reduce the incidence of unwanted side effects (e.g phrenic nerve block)
Open surgery may need additional superficial cervical plexus block or surgical infiltration